The world is in desperate need of protective gear to keep health care workers safe and ventilators to help severely ill COVID-19 patients breathe. In the face of massively increased demand and stalled supply chains, engineers are scrambling to redesign equipment so it can be produced outside of specialized factories.
Researchers at academic institutions are drawing on the spirit of the independent maker movement, according to Saad Bhamla, a bioengineer at the Georgia Institute of Technology. “We’re tapping into this whole existing community,” he says, noting that many cities have clubs for DIY enthusiasts. Such individuals often volunteer their time at fabrication labs and maker spaces. Now the COVID-19 pandemic is presenting them with a unique problem. “People have a call to arms,” Bhamla says, “and they’re tapping their creative and problem-solving abilities.”
The do-it-yourself approach is most evident in the case of face masks: hobbyists are sharing designs and instructions that allow amateurs to sew their own washable coverings. Some are donating these masks to hospitals, though in a medical setting, such unofficial gear can only serve as a last resort. Previous research has shown that while homemade facial protections can reduce the spread of microbes, they are less effective than professionally produced surgical masks. This disparity is in part because surgical masks are made from materials that are better at halting the virus-carrying droplets that spray out when humans sneeze and cough than fabrics such as cotton, which is used in many homemade versions. Instead of relying on contributions from individuals, some hospitals are sending medical-grade materials to a variety of clothing manufacturers, from fashion designer Christian Siriano to an Amish community in Ohio, who have begun mass-producing more impermeable masks and gowns.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
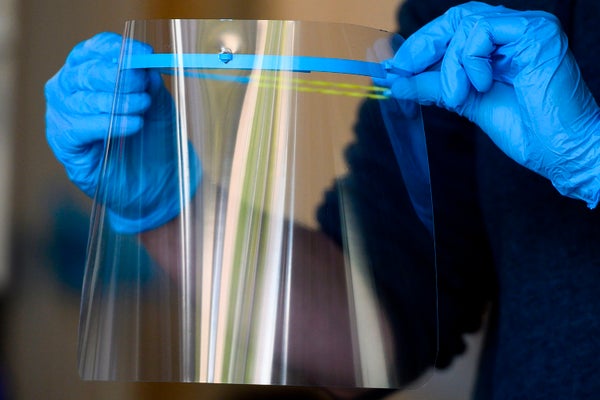
But masks are only one element of the personal protective equipment that health care workers need—and they do not require a redesign for sewing machines to manufacture them en masse. Gear such as face shields—transparent plastic sheets that wearers strap to their forehead to provide an additional barrier against droplets—are another story. It is possible to MacGyver such a device from a sheet of plastic and zip ties or rubber bands, but the process and results would be too time-consuming and ill-fitting for mass production. Instead engineers have come up with several ways to make facial shields that 3-D printers and laser cutters can churn out.
Facial Protection
Bhamla is a member of one of the first teams taking a DIY approach to coronavirus equipment, which is coordinated on the business communication platform Slack. When Nicholas Moser first joined the group, called Helpful Engineering, he says it had roughly 300 participants. As its focus shifted to coronavirus-fighting designs, membership ballooned to thousands at the time of this writing. Moser, who has experience as a project manager, became lead of MASKproject, a subgroup that aims to develop protective gear. MASKproject quickly began refining two face shields, eventually focusing on an origami-style design. Any commercial die cutter, laser cutter or water jet can slice the open-source design from a flat sheet of plastic, which is then folded by hand into the appropriate three-dimensional shape.
Moser says his team’s face shields are already going out to five hospitals, including ones in New Orleans, Massachusetts and California, at a rate of about 10,000 per week. Other organizations have followed: both the Massachusetts Institute of Technology and Duke University Health System have announced that their researchers developed and tested their own face-shield prototypes. Like the MASKproject’s design, M.I.T.’s shield is produced on a die-cutting machine and then folded by hand, whereas Duke Health’s uses a 3-D-printed headband.
In all these cases, the new shields can be produced on relatively common machines—laser cutters, die cutters and 3-D printers are found in many maker spaces, labs and production facilities that do not typically make medical equipment. Moser’s team wants to work with a variety of partners to produce its devices, he says. “Everything from a small shop that does letterpress—that cuts out pieces of paper in shapes—to large factories that have roller die cutters that can produce hundreds of thousands [of shields] a day,” Moser adds. Devices churned out by this so-called distributed-manufacturing model then flow to a central hub for quality control and sanitization before they are shipped to hospitals. “Part of this project, which is fascinating, is that there’s never been this sort of distributed manufacturing,” he says. “This scale of distributed manufacturing has never been done. And the supply chains are getting worked out amazingly rapidly, with all these people.”
In Need of N95s
Although distributed manufacturing has the advantage of speed, it requires reengineering equipment so that items can be produced with machines such as 3-D printers rather than specialized devices. And not all the new designs meet strict medical standards, which are particularly important for major items that are now seriously scarce: N95 respirators. Surgical masks can halt droplets, but viruses can still squeeze through the material. This possibility is a concern when the air gets filled with viral particles, which happens when doctors ventilate severely ill coronavirus patients. To protect themselves in such situations, medical professionals don N95 respirators. These masks fit snugly to the skin, only admitting air through a dense filter that blocks 95 percent of very small particles while still allowing wearers to breathe without undue effort.
The filter within an N95 is made of spun polypropylene, a material currently in short supply. So Moser and his colleagues are designing a similar device that can employ other substances. “We have designed and prototyped and are testing a filter-agnostic face shield to be an alternate to N95,” he says. The MASKproject respirator consists of a 3-D-printed base that can fit tightly to the face. The product has a front grate that forces air to enter through a stack of filtering materials, including high-efficiency particulate air filters “that meet the same particle specification as the N95. So they’re not rated for being used like this, but they have a similar classification,” Moser says. His group is currently testing the devices for both filtering and breathability.
MASKproject’s device is unlikely to jump through all the regulatory hoops that certified N95 respirators must pass, however. “Products like N95 respirators do go through a stringent testing process to be qualified at that level,” says Julie Swann, a professor of industrial and systems engineering at North Carolina State University. But the current pandemic will not wait for testing: the Food and Drug Administration recently announced that in emergency situations, U.S. organizations can turn to substitutes such as KN95s, comparable protectors used in China. Moser sees his team’s alternative to N95 as a similar backup option. “MASKproject, myself and Helpful Engineers—we’re not making medical devices,” he says. “We’re making general-use products that we are testing to the same international standards as the comparable devices that are in short supply. But they’re not certified, and they’re not regulated, and they’re not meant for medical use.” Moser notes that hospitals can request MASKproject’s devices, “but they’re not being marketed for medical use at all.” Despite this disclaimer, he says, his team is pursuing certification from the FDA and the National Institute for Occupational Safety and Health at the U.S. Centers for Disease Control and Prevention.
Ventilator Redesign
Like N95 respirators, ventilators must meet extremely strict standards. When the amount of oxygen in COVID-19 patients’ blood drops to dangerous levels, these machines attempt to breathe for them. But the complex, expensive devices are in limited supply all over the world, even as manufacturers increase their rate of production.
“In the U.K., the issue is that our ventilator manufacturers are fantastic—but current capacity to manufacture is about 2,000 per year,” says Mark Thompson, an engineer at the University of Oxford. He notes that the country will need many more machines than that in order to support the estimated number of COVID-19 patients who will require them in the coming months. “It’s just not possible to scale the production of any one of our ventilator manufacturers,” he says. “It needs to have a completely different solution.”
Thompson is one of several researchers spearheading the development of a single-use ventilator substitute inspired by an existing product: the squeeze bag that health workers employ to manually control a patient’s breathing in emergency situations. With an oxygen supply and an apparatus to automate the squeeze-and-release process, such a device could help an infected person breathe for a prolonged period of time in a way similar to a ventilator. In this case, Thompson’s team wanted to achieve that automated process with off-the-shelf parts to make the device easier to manufacture. “Essentially, it revolves around this idea of having lots of single-use items [that] are widely available [and that] are all patient-facing pieces of equipment,” he says. After a breakneck two-week development period, Thompson and his colleagues began testing their ventilator substitute, called OxVent. And they are currently in the second round of testing to secure approval from the Medicines and Healthcare Products Regulatory Agency, a U.K. body akin to the FDA in the U.S. Once the developers get the green light, they plan to have medical device manufacturer Smith+Nephew produce their open-source design.
OxVent was an early entry in the race to redesign ventilators for faster manufacturing, but it is not the only contender. Three different groups of physicists have developed their own emergency ventilator prototypes. And this month the CoVent-19 Challenge launched an open contest calling for new ventilator designs. The plan is that they will be developed over the course of only two months.
These designs will not be as sophisticated as regular ventilators. For example, Thompson notes that his team’s product will have to be discarded after it is used on a single patient. It will also lack the monitoring equipment and alarms that full-scale ventilators have. On the other hand, companies will be able to scale up production of emergency ventilator designs much more quickly by using the type of distributed manufacturing that Moser’s work also relies on. “The challenge is to [make] an additional number of about 20,000 ventilators before the peak of the epidemic,” Thompson says. “We think that with that kind of distributed system, we have a chance of managing to do that.”
Read more about the coronavirus outbreak here.